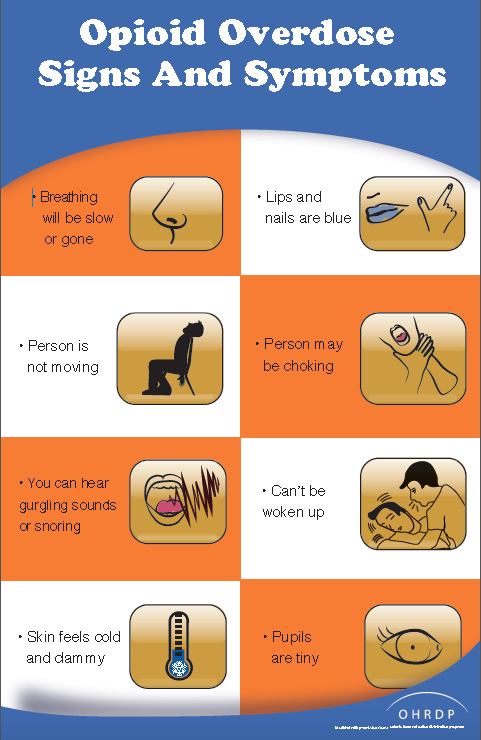
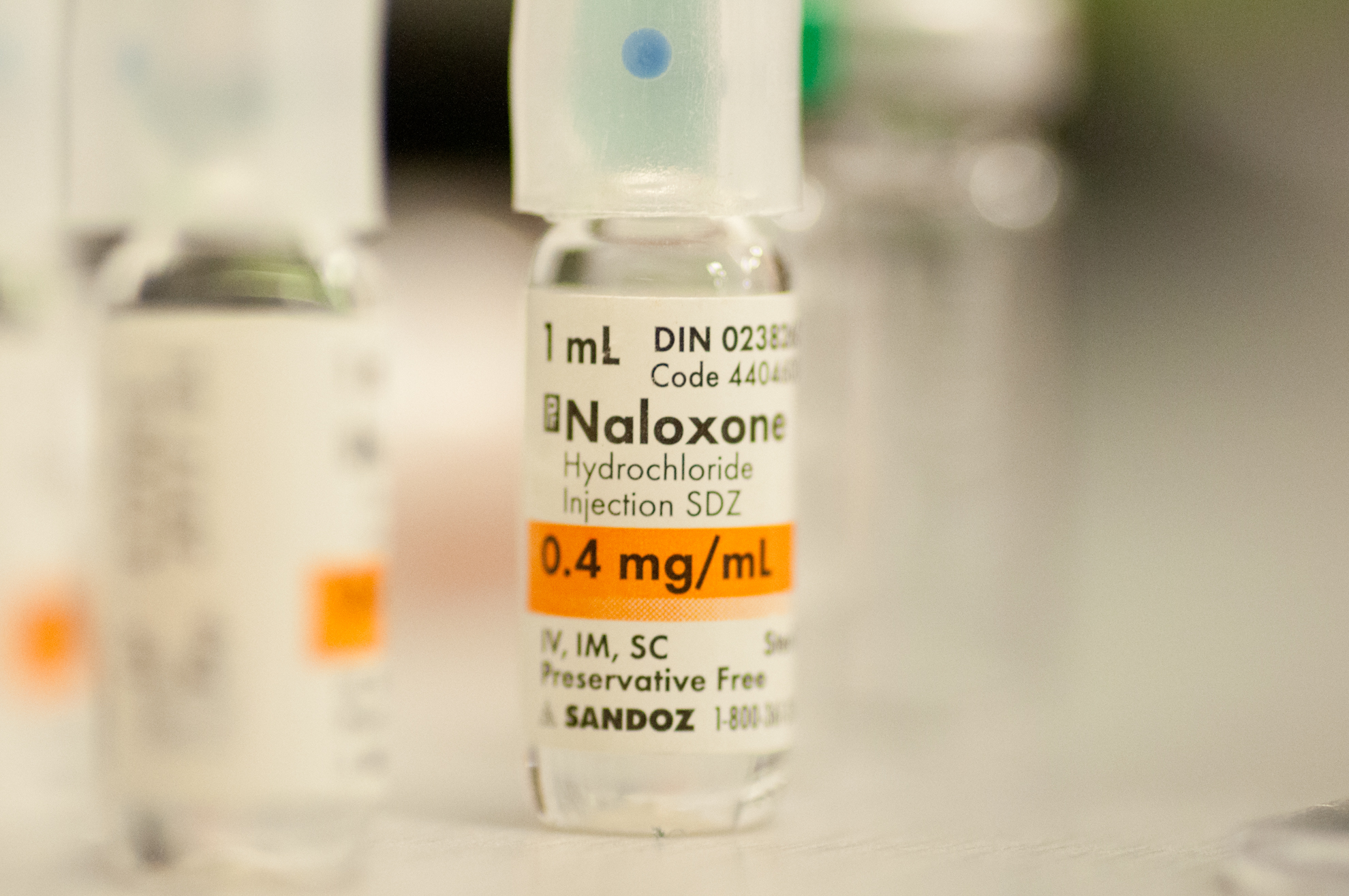
This page contains information on the signs and symptoms of opioid overdose, Naloxone spray and Naloxone intramuscular injection information.
Naloxone is a temporary antidote for opioid overdoses, including those caused by Fentanyl. When properly administered it can restore normal breathing and consciousness to individuals experiencing an opioid overdose.
Because the depression of breathing caused by opioids can last longer than the action of Naloxone, further treatment in hospital is required. Naloxone is available in both spray and intramuscular injection kits.
For more information visit: http://towardtheheart.com/fentanyl/
Product Purchasing Information for First Responders: http://adaptpharma.com/products/
After you have assessed the situation, and concluded that the individual is suffering from an opioid overdose and requires naloxone you must:
- Wear appropriate PPE as the situation dictates;
- Following the assessment at the scene, determine the best way to reposition the individual, removing them from the toxic area or source of exposure if possible (i.e., to fresh air), in order to prevent further exposure. Ensure that other hazardous objects are not in close proximity to the individual to prevent any harm to themselves or the first responders; and
- Reposition the individual on their back;
- If the individual is not breathing or has no pulse, start CPR.
- If you are not with a co-worker, complete one full cycle of CPR prior to administering the first dose of naloxone; or
- If you are with a co-worker, one First Responder should perform CPR while the other administers naloxone.
- Be aware of other sources of contamination before providing rescue breathing.
- Always use a one-way valve pocket mask to provide artificial respiration. Do NOT perform direct mouth-to-mouth resuscitation. Note: ensure contaminates on the face are covered by the one-way valve pocket mask.
Note:
After the patient assessment and a decision is made to rescue breath, oxygen should be added along with ventilations when available by a trained first responder.
Patients with opiate overdose who are in cardiac arrest are so because of acute hypoxia. It is critical to begin chest compressions, ventilate and oxygenate these patients if restoration of spontaneous circulation is to occur.
- Lay the individual on their back in order to appropriately administer a dose of naloxone nasal spray.
- Remove the naloxone nasal spray from the box.
- Peel back the tab with the circle to open it.
- Hold the naloxone nasal spray with your thumb on the bottom of the plunger and your first and middle finger on the side of the nozzle. Do not press the plunger to test – If you do, you will waste part or all of the medication.
- Tilt the individual’s head back and provide support under their neck with your hand.
- Gently insert the tip of the nozzle into one nostril until your fingers on either side of the nozzle touch the individual’s nose.
- Press the plunger fully to give the full dosage of the naloxone nasal spray.
- Remove the device from the nostril after giving the dose.
© 2016 ADAPT Pharma, Inc.
After administering Naloxone, continue delivering Artificial Respiration (AR) or CPR. Use a one-way valve pocket mask to provide artificial respiration.
After 2-3 minutes if there is no responsiveness (no breathing/no pulse/unresponsiveness), or the individual responds but then relapses into respiratory depression, administer another dose of naloxone using a new nasal spray in the opposite nostril.
If the individual starts to breathe, AR/CPR and naloxone administration is no longer required. Place them in the recovery position and await EMS. They must be provided with further medical assistance. If the individual starts to breathe and regains consciousness, provide constant reassurance that further medical support is on its way.
Once the EMS arrives, indicate the number of naloxone doses given and provide EMS with the used nasal spray bottles for disposal/destruction at the hospital. The used naloxone spray device is considered to be a biohazardous material and must be handled as such.
Remember to remove your PPE while exercising universal precautions.
- Naloxone nasal spray must be stored at room temperature between 15°C to 25°C (59°F to 77°F)
- The naloxone needs to be readily accessible (i.e.: located in a pocket or pouch rather than in a vehicle).
- The issued naloxone nasal spray must be maintained in good functional condition.
- Do not prime or test the device.
- Notify your supervisor if the naloxone unit seems damaged or defective, missing or expired/near expiry.
- If your naloxone kit is personal issued, ensure that you store it as per the manufacturer instructions when at home and keep out of the reach of children.
- Do not freeze naloxone nasal spray. Protect it from light.
OTHER INFORMATION
First responders should consult with either their health services or personal health care providers for any health related questions they may have about having naloxone administered to them.
Report any suspected side effects related to the use of naloxone nasal spray to Health Canada by calling 1-866-234-2345. For medical advice, visit your healthcare provider.
Naloxone nasal spray is not intended for self-administration.

For assaultive behaviour, individuals who are opioid dependent have a high likelihood of presenting assaultive behaviour upon regaining consciousness. Be prepared to deal with a potentially assaultive subject after the administration of naloxone.
Although highly unlikely for operational members to experience precipitation of severe opioid withdrawal, they may unintentionally exhibit assaultive behavior upon regaining consciousness.
- Be aware individuals may become assaultive when administered naloxone
- Remove any objects the individual may reach for use against themselves, yourself, or anyone in the vicinity
- Follow use of force guidelines to keep control of the situation
For convulsions,
- Ensure that objects that could cause injuries are moved away
- Protect the individual’s head with blankets or other soft materials
- Keep other dangers away from the individual
- After the convulsions stop, place the individual in the recovery position
- Keep the individual comfortable and warm
For diarrhea,
- If there is external soiling, avoid contact with the fecal matter
- Consider covering the fecal matter in order to minimize the exposure
- Wash your hands with soap and water at the earliest opportunity
For vomiting,
- Individuals experiencing precipitation of severe opioid withdrawal have been known to experience projectile vomiting
- If the individual begins to vomit, roll them in the recovery position to protect the airway
- Avoid contact with bodily fluid
- Keep them in the recovery position, as instructed through First Aid Training, and clear their mouth of any blockage (ensure to wear gloves)
- Wash your hands with soap and water at the earliest opportunity
Risk of Cardiovascular (CV) Effects:
Abrupt postoperative reversal of opioid depression may result in adverse CV effects. These events have primarily occurred in patients who had pre-existing CV disorders or received other drugs that may have similar adverse CV effects.